Findings could pave the way for innovative treatments
By Amy Ratner, director of scientific affairs
Results of research funded by Beyond Celiac point to a more precise way that gluten sets off damage to the intestine in those who have celiac disease and could help in the development of innovative approaches to finding a treatment.
The study, by Arnold Han, MD, a gastroenterologist at Columbia University and recipient of the Beyond Celiac/Society for the Study of Celiac Disease Early Career Investigator grant, describes the way gluten triggers two kinds of T-cells to coordinate and cause damage.
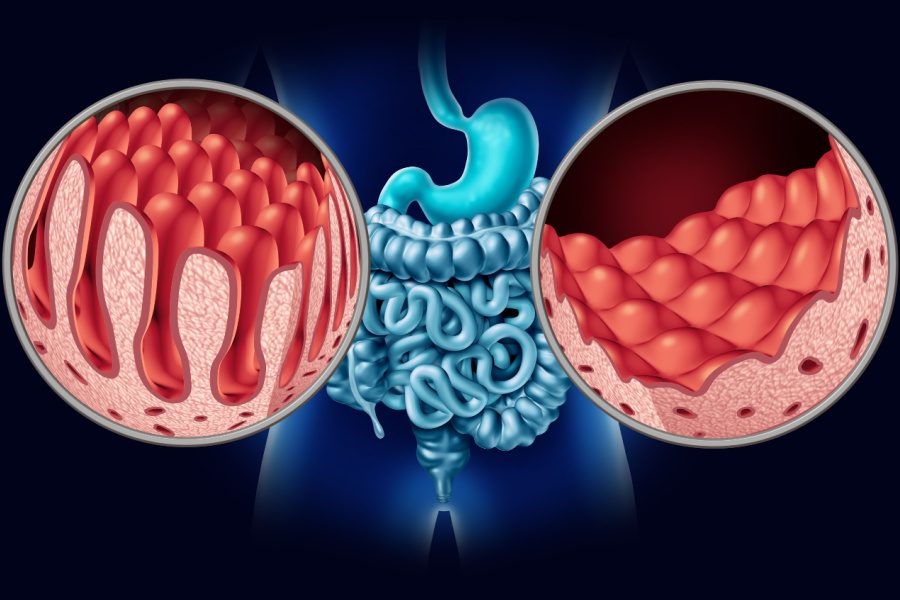
T-cells are white blood cells that function as the body’s disease fighting soldiers and are part of coordinated immune system battle. In the case of celiac disease, these soldiers incorrectly read gluten peptides as the enemy, rally the immune response troops and go on the attack, with resulting destruction of the absorbing lining of the intestine.
The new study, published in the journal Science Immunology, provides important clues about the way CD4 T-cell responses to gluten ultimately lead to intestinal damage by intraepithelial lymphocytes. Intraepithelial lymphocytes are T-cells found in the intestinal tract.
“We show that gluten somehow induces rapid and deliberate activation of the [intraepithelial lymphocytes],” Han said.
This was somewhat unexpected because the intraepithelial lymphocytes are not thought to recognize gluten on their own, he noted. The study suggests that these cells shift from anti-inflammatory defenders to pro-inflammatory attackers, leading to intestinal damage.
Evidence from the study, which is ongoing, could be used in the development of new treatments for celiac disease based on what it reveals about the way that gluten causes the immune reaction in celiac disease.
“An improved understanding of any disease process can inform new avenues for therapy,” Han said. Many celiac disease drugs currently being developed focus on the activation of the CD4 T-cells, but this new research with its improved understanding of how the intraepithelial cells are activated could contribute to treatments that target them, he noted.
Han and colleagues at Columbia University analyzed T-cells from the intestinal biopsies of 37 study participants in three categories — 11 with who had just been diagnosed and were considered to have untreated celiac disease, 19 with active celiac disease on a gluten-free diet and seven with potential celiac disease who had positive blood tests for celiac disease antibodies by no damage to the intestine. The study also included 17 participants who did not have celiac disease.
Study participants in all three categories of celiac disease had an enriched number of intestinal T-cells, including CD4 helper cells, regulatory T-cells and CD8 intraepithelial cells.
Blood samples from study participants who had been on a strict gluten-free diet for at least six months and volunteered to eat four slices of gluten-containing white bread per day for three days, a gluten challenge, were also analyzed.
In celiac disease, although intestinal damage can heal completely on a gluten-free diet, changes in the intraepithelial cell population can persist for years, Han said. These persistent cells have distinct T-cell receptors and researchers are working to understand what the receptors are recognizing if it is not gluten. The receptors on the surface of T-cells play a significant role in immune response by activating the cells to respond to antigens, acting as a kind of warning system alarm switch. An antigen is a marker that tells your immune system whether something in your body is harmful or not.
In celiac disease, gluten is the antigen recognized by CD4 T-cells. “However, we don’t know the antigens for these intraepithelial cells that appear to cause damage,” Han noted. Previous research done by Han suggested that microbial antigens, which are microorganisms including bacteria, viruses and more, or self-antigens, which are normal substances found in a person’s body, are potentially being recognized by the intraepithelial lymphocytes.
The new study found that groups of cells that shared the same T-cell receptors, called T-cell clones, which were present in the intestinal biopsies of study participants with celiac disease were later seen in the blood following the gluten challenge. Researchers were able to track how a given T-cell clone behaved and found that the T-cells in the intestine were changing to become more inflammatory in the blood, Han said.
In ongoing research Han and colleagues are aiming to better understand how intraepithelial cells are activated by gluten. His research will also include study of celiac disease using organoids, tiny three-dimensional mini organs grown in a petri dish from the intestinal cells of celiac disease patients.
You can read the study here.
CD4 T-cells
CD4 cells, also known as CD4 T lymphocytes or “helper T cells,” belong to the category of white blood cells. In a healthy person, their primary function involves aiding the immune system in combating infections by stimulating the destruction of viruses, bacteria, and other harmful microorganisms that could potentially cause illnesses.
Intraepithelial lymphocytes
Intraepithelial lymphocytes (IEL) are special immune cells found in the lining of the intestines, respiratory tract, urinary and reproductive tracts, and skin. Their main job is to be the first line of defense against harmful germs or pathogens that enter these areas through the surface.
Regulatory T-cells
Regulatory T cells (Tregs) are a special type of T cells that have a unique job in our immune system. In a healthy person, they work to control and limit the immune response to keep everything in balance and make sure our body doesn’t attack itself by mistake. Tregs can stop other T cells from growing too much and producing too many signaling molecules (cytokines) that can cause harmful reactions. Because of this, Tregs play a crucial role in preventing our immune system from mistakenly attacking our own tissues and causing autoimmune diseases.
CD8 intraepithelial lymphocytes
CD8 intraepithelial cells, also known as CD8+ intraepithelial lymphocytes (IELs), are a specific type of immune cell that plays a crucial role in the immune defense of the GI tract. Their main function is to survey the intestinal lining for signs of infection, tissue damage, or cellular abnormalities. They are involved in maintaining the integrity of the intestinal barrier and promoting tissue repair after injury or inflammation.
T-cell clones
T-cell clones are an essential part of the immune response, as they allow the immune system to amplify the number of T cells capable of recognizing and attacking a particular invader. This clonal expansion results in a stronger and more targeted immune response against the invading pathogen or abnormal cells.
Opt-in to stay up-to-date on the latest news.
Yes, I want to advance research No, I'd prefer not to